News A new and non-invasive way to test early for the often-debilitating condition has been developed by Australian researchers. The validity of using blood tests to diagnose endometriosis is currently being tested for clinical use. A non-invasive and cost-effective blood test could transform the way endometriosis diagnosis is carried out, potentially changing how GPs are […]

News
A new and non-invasive way to test early for the often-debilitating condition has been developed by Australian researchers.
A non-invasive and cost-effective blood test could transform the way endometriosis diagnosis is carried out, potentially changing how GPs are involved.
Promising new research, published in the international journal Human Reproduction, demonstrated ‘strong predictive accuracy’ for the diagnosis of endometriosis through a blood test.
The research was developed by Perth-based medical technology company Proteomics International, in collaboration with the Royal Women’s Hospital and the University of Melbourne and analysed plasma samples from 805 participants across two independent groups.
Professor of Women’s Health Research at the University of Melbourne Peter Rogers said this ‘breakthrough is an exciting advance in the diagnosis of this debilitating disease’.
‘These results are a significant step towards solving the critical need for a non-invasive, accurate test that can diagnose endometriosis at an early stage as well as when it is more advanced,’ he said.
Associate Professor Magdalena Simonis, a GP with a special interest in women’s health, told newsGP the findings were very promising, but GPs will still need to be aware that this test, if it becomes integrated into general practice, will not be a blanket solution.
‘We must always keep a focus on the symptoms that a woman presents to us with, so that we don’t become blindsided by particular results, especially when we’re dealing with new testing,’ she said.
‘It might be a prohibitively expensive test – so it needs to be affordable, it needs to prove to be accurate and it needs to also give women an option to proceed with further investigations if that’s deemed necessary.
‘I expect that we will use this as a support to our investigative tools.’
According to the Australian Institute of Health and Welfare, the condition, which affects at least one in nine women and girls, currently has a diagnosis delay of seven years and has been estimated to cost the economy over .4 billion a year.
Associate Professor Simonis said she hopes that a blood test could shift the role that GPs play in this space.
‘This shifts that diagnostic timeline back to general practice, which is a first for endometriosis,’ she said.
‘It doesn’t take us away from some of our other primary concerns, which is increasing consumer and patient literacy and understanding around menstrual cycles and what is outside of the norm.
‘We need to keep reminding women and our colleagues that any symptoms that interfere with a person’s ability to function to their full capacity or stop them from going to school or work, needs to be further investigated whether it turns out to be endometriosis or not, that doesn’t necessarily address the issues of other causes of chronic pelvic pain or heavy menstrual bleeding.’
Proteomics International’s Managing Director Dr Richard Lipscombe said the identified protein biomarkers, or ‘fingerprints’ in a patient’s blood, could be identified ‘from as early as when they start having periods’.
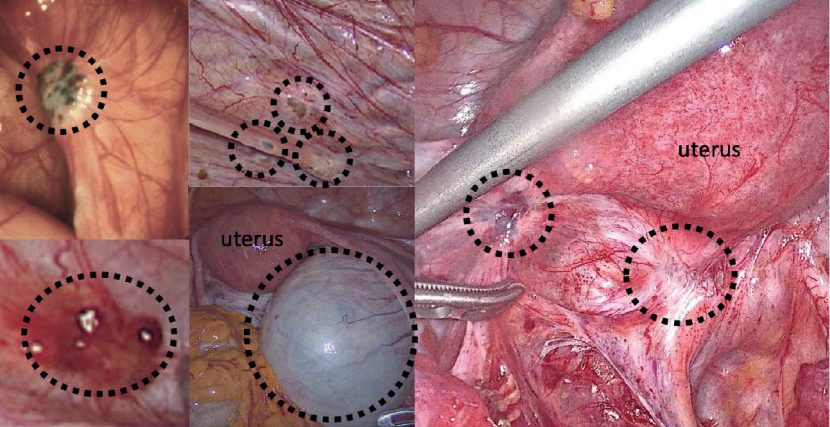
‘A blood test is more cost-effective for patients and the health system than the current use of ultrasounds, invasive laparoscopies, MRI’s and biopsies to diagnose endometriosis, and work is underway to fortify the robustness and reliability of the new test for clinical use,’ he said.
Although the early results indicate confidence in the research, Associate Professor Simonis still wants to see how this plays out when translated into a clinical environment.
‘Science is one of those really tricky areas where until you actually put something into practice and test a cohort ethically, you will not be able to make that evaluation with confidence that it can be generalized to the rest of the population, because we do know that there are also ethnic differences in menstrual cycles,’ she said.
‘But it might actually have a really positive impact on reducing hospital waiting times and I think for rural and remote women, who don’t have access to the services that we have in metropolitan areas, it could make a very big difference to our marginalised patients.’
Log in below to join the conversation.
chronic pain endometriosis preventative health scope of practice women’s health
newsGP weekly poll
How do you rate the value that your Primary Health Network provides?