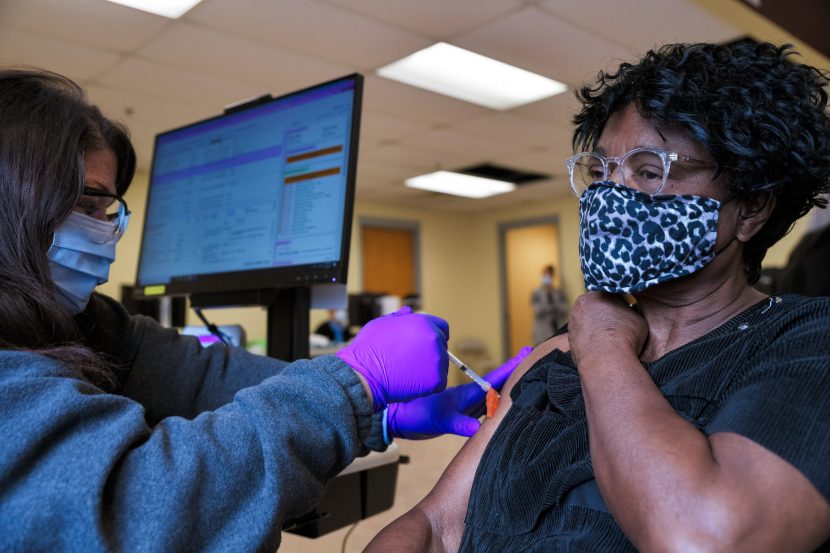
The study, which was published in the Journal of Health Psychology, looked at how patients with Long Covid experience their illness. The study found that many patients feel they have to prove their illness is physical to be taken seriously and, as a result, often reject psychological support, fearing it implies their symptoms are “all […]


The study, which was published in the Journal of Health Psychology, looked at how patients with Long Covid experience their illness. The study found that many patients feel they have to prove their illness is physical to be taken seriously and, as a result, often reject psychological support, fearing it implies their symptoms are “all in the mind”.
Saara Petker, clinical psychologist, co-author of the study and former PhD student at the University of Surrey, said:
“We found that our participants are living a life of constant uncertainty, struggling to find treatment. People told us that they didn’t feel listened to, some said they’d lost trust in doctors, their social circles and even their own bodies because of the whole experience.
Petker, S., & Ogden, J. (2025) Patients’ experiences of living with Long Covid and their beliefs about the role of psychology in their condition. Journal of Health Psychology. doi.org/10.1177/13591053251325112.
“Medical advice is crucial – but psychological support must be offered with care. If it’s seen as replacing medical help, it can feel dismissive.”
According to the Office for National Statistics, there are 1.9 million people who live with Long Covid in the UK. Long Covid symptoms include fatigue, difficulty concentrating, muscle aches and shortness of breath, which persist for many weeks, sometimes months, after the initial Covid-19 infection.
We found that the problem isn’t people with Long Covid refusing help – it’s about the deep need for people to be believed. When a patient feels dismissed, offering psychological support instead of medical care can be misconstrued as insulting.”
Jane Ogden, Professor, University of Surrey