A wearable pulse oximeter and connected software platform show promise for monitoring obstructive sleep apnea (OSA) and other sleep-related breathing diseases, according to research presented at the ATS 2025 International Conference.
The device (pulse oximeter), which is cleared for medical use, was designed for comfort and ease of use; a clinical trial found high rates of utilization by patients. It could be used to track patient response to OSA treatment over time.
Investigators in our clinical research trials report how useful longitudinal data are to observe night-to-night variability and the response to treatment of OSA. One sleep specialist even reported that it may be better to collect one or two channels of data over 25 nights than 25 channels over one night, which is considered the gold standard with in-lab polysomnography.”
Ketan Mehta, MS, head of product and engineering for Connected Wearables at Apnimed
Wearable sensors like the Oura ring and Apple Watch that measure biometrics during sleep are widely used by consumers, but are not cleared for medical use. At the same time, other medical devices used in sleep studies gather clinically relevant data, but are too cumbersome and costly to use for frequent monitoring. This tool could potentially expand patient access to care through pulmonologists to manage routine sleep apnea in their patients, instead of having to refer them out to a sleep specialist, he added. The device provides a bridge between these two extremes, he said.
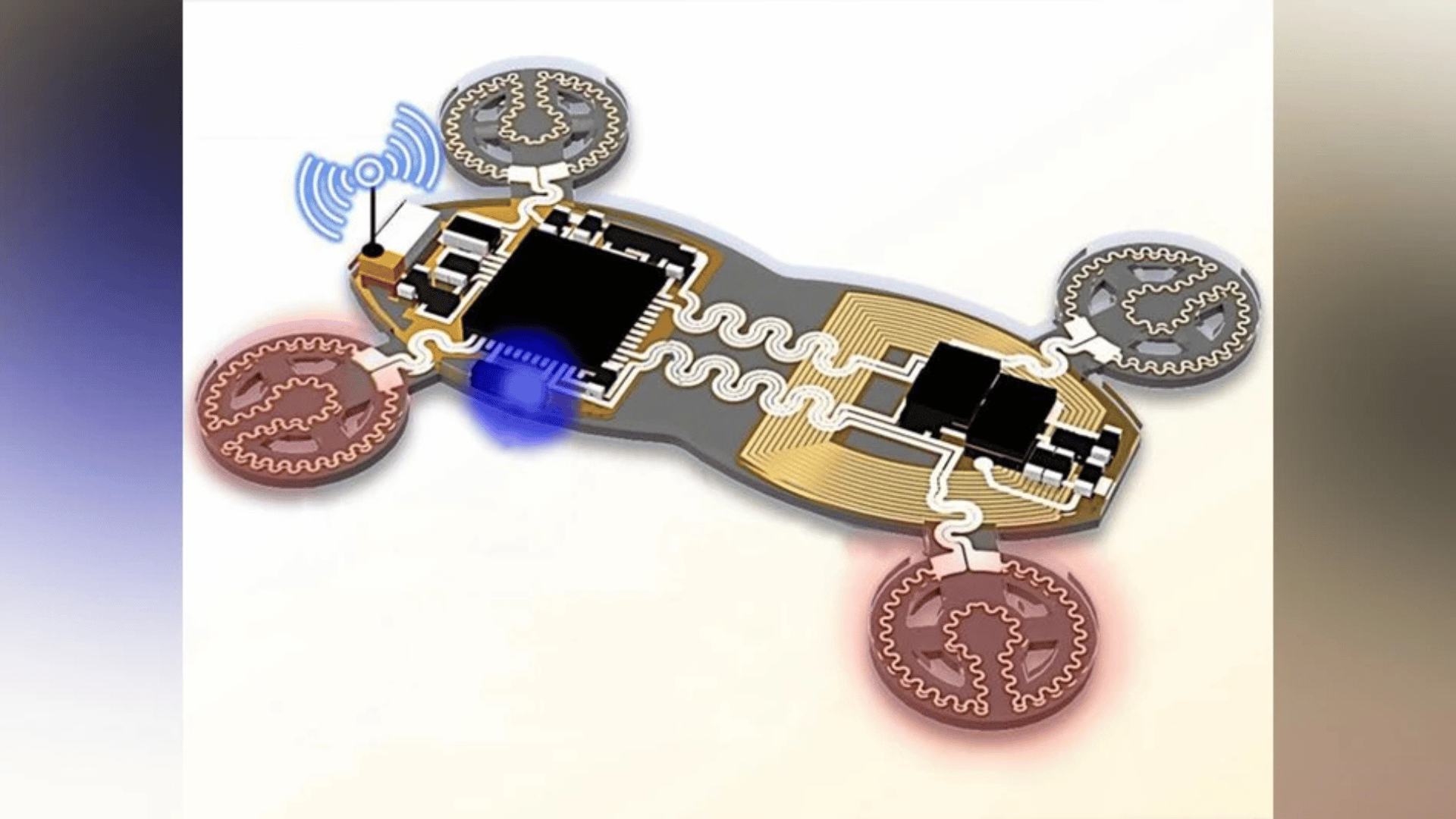
Worn as a ring, the device offers several key differences from other consumer wearables. Notably, it uses transmittance-based photoplethysmography, which has been shown to be more suitable for the proximal phalanx region, provide better signal-to-noise ratio, and is more effective in low perfusion situations. It also engages in continuous data collection, rather than spot checks, he added.
The device connects to an app that users can access from their smartphone, giving patients access to a subset of the same data as their health care providers.
“These data empower both parties to be informed, and they’re able to have more meaningful conversations. This offers the opportunity for shared decision making between patient and provider using digital medicine,” Mr. Mehta said.
The device was used in several different clinical settings including to monitor patient response to a pharmacologic treatment program for OSA. During the monitoring study, patients were asked to wear the device for 9 nights over a 47-day period. However, many patients voluntarily wore their devices more often, with 85 percent of patients using beyond the recommended nights. One patient used the device almost nightly for 44 days, the researchers noted.
In addition to clinical use, the device and connected software could be applied to research in conditions like COPD, ILD, and other conditions that involve sleep-related breathing diseases and require monitoring of oxygenation, noted Mr. Mehta. The device is FDA cleared for medical use; the connected software requires similar clearance before it can be deployed outside of clinical trial settings
Researchers hope to continue gathering data to further validate use of the device and connected software and better understand the patient and clinician experiences, the team said.
Source:
American Thoracic Society